Osteocartilage degeneration in the lumbar spine is a malnourished spinal disease in which the normal structure of the entire spine and intervertebral disc is gradually destroyed.It should be said that not only the back suffers, but also the entire organism, especially the pelvic organs and lower limbs.
Reasons for development
The waist area of a person's waist is associated with directness and cannot be fully compensated even if the large size of the vertebrae is.Therefore, the slightest change in the human body, the reduction of muscle corsets on the lower back, excessive weight, injury, incorrect exercise, etc. may lead to the development of the disease.Also, you should always remember the age-related changes in everyone’s spine.
By summarizing the above, the most common risk factors can be distinguished, with the total number leading to lumbar skeletal disorders:
- Uneven and irregular loads on the spine (increasing severity from the inclined position, etc.).
- Too much weight (almost every kilogram is important).
- Rumber was injured, including exercise.
- Weakness of muscle corset (long-term work in monotonous position, etc.).
- A poor fusion diet, minerals and vitamins.
symptom
However, the symptoms of the disease can be very large, however, generally forming an overall image of the main signs of osteochondrosis in three syndromes:
- Vertobrogenous Lumbalgia (synonym Lumbago).
- vertro-carbon lumbar behavior.
- vertro-Carbon ischemia (inflammation of sciatic nerve).
However, in addition to pain in the waist area (leg radiation, hips, groin area or absence), tension in the lower back muscles, weakness in legs, tightening in lower back movement, and difficulty in waist movement should be distinguished by other important symptoms of lumbar granulocyte inflammation.
- The legs are numb, and the chicken skin crawling on the legs is crawling.
- Cramps on the legs.
- Pelvic disease (later of urine, constipation or diarrhea or urinary incontinence).
- Weaknesses in certain leg muscles.
These complaints can enable neurologists to have a level of damage to the spine and to make a differential diagnosis through other spinal diseases.
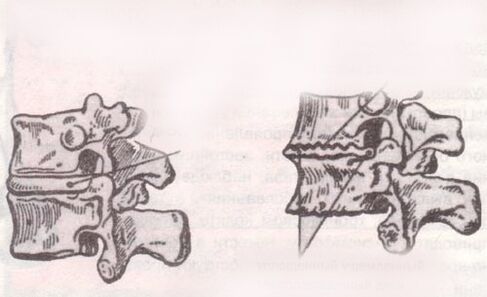
Diagnostic and X-ray markings

Osteochondrosis should have only one type of instrumental method - radiology.Visualizing the entire structure of the spine in modern medicine allows for optimal MSCT or MRI studies, however, simple radiography does not lose its estimates (as a screening study).It is important to remember that the main stage of diagnosing a spinal problem will be a medical test, and sometimes you can make a diagnosis without the test at all.
In the nervous state, pain is found when palpating the spicy process of the vertebrae, tension of the lower back muscles, and if only osteochondral bone disease is not the symptoms, such as tendon reflexes, impaired sensitivity, impaired symptoms, signs of movement of movement (signs of weak movement), especially signs of movement of movement of legs.In the presence of these symptoms, differential diagnosis of disc herniation and other more serious spinal diseases should be performed.
treat
Treatment of the disease involves long-term complete treatment.Directions of treatments for multiple drugs - non-drug-assisted approaches and preventive physical therapy practice methods, used in part during the acute period and has not lost relevance to today.
drug
It is a combination of fibroid treatment, anti-inflammatory pathogenic therapy, and the use of neuroprotective drugs.The choice of drug and dosage calculations begins with a person's weight, gender and the presence of concomitant disease.
In acute periods, it is recommended to inject drugs such as diclofenac and meloxicam.Similarly, at the same time, they began treatment to clear out muscle cramps and protect nerve fibers from damage.
Non-drug

It is represented by physical and manual influence.Given the mass of the muscle groups, the anatomical area is quite extensive, and physical chemistry can only be an auxiliary method.Using DDT, electrophoresis, and magnetic therapy can enhance the effect of the drug.
But even without medication support, massage and manual therapy can sometimes completely prevent the symptoms of osteochondrosis in the waist.This is due to the fact that muscle cramps are well removed and that pain is not always caused by the inflammatory process, and sometimes only careless exercise can lead to pain, effectively eliminating the pain within the first few hours after the pain develops.
Gymnastics of osteocartilage degeneration in the waist area are designed to stretch the muscles of the back and strengthen them.In the case of a given diagnosis, lumbar osteochondrosis should be performed daily physical therapy exercises.Following general rules (restricting excessive hypothermia), weight control and exercise on osteochondrosis in the waist area can sometimes be forgotten for years.
























