In the pathological structure of the bone-joint system, osteoarthritis predominates - about 70% of cases belong to its share. People after age 50 experience similar problems most often, but the first signs of the disease appear even in younger people. The disease has serious medical and social implications, as in many cases it can be a cause of working-age insufficiency.
Many people are aware of a pathology like arthropathy, but not every patient understands why it develops, how it manifests, and what it takes to fight the disease. Increased awareness and caution can prevent harmful changes from occurring and developing.
reason
Osteoarthritis is characterized by a degenerative dystrophic process in all joint tissues: cartilage, subchondral bone, ligaments, muscles and tendons. The disease is considered one of the "partners of aging" because it often affects older patients. But age is far from the only cause of joint deformities. The origin of the disease is very heterogeneous and is due to pathological effects on the external and internal types of the body.
For every patient, there are certain risk factors that contribute to the development of joint disease. Therefore, the causes of arthropathy combine the following conditions:
- Hard physical labor.
- Inactive.
- trauma.
- Joint dysplasia.
- Inflammation (arthritis).
- overweight.
- Menopause estrogen deficiency.
- Thyroid disease.
- Consequences of joint surgery.
- hereditary.
As you can see, the development of arthropathy is mediated by heterogeneous factors, which in most cases are of a mechanical or exchange nature. In this case, the patient's lifestyle and their occupation are very important, since loaders, manual workers and athletes often suffer from arthropathy.
Arthropathy has a variety of causes and is characterized by local effects on the joints and general effects on the body.
development mechanism
The normal function of the joint is ensured by the harmonious working of all its structures. But the main component of any joint is cartilage. It provides shock absorption and resists stress on the joints. Cartilage tissue is composed of cells (chondrocytes) and a matrix, the main substances of which are proteoglycans and collagen.
If the load on the joint exceeds the allowable range, the first is the structural disorder of the cartilage. The proteoglycans that hold collagen chains are lost, which increases the sensitivity of the tissue to external influences. The destruction process begins to outperform synthesis. This is facilitated by reduced cartilage nutrition when synovial fluid contains insufficient amounts of nutrients. Inflammatory responses and hormonal imbalances support imbalances in tissue turnover.
All of these cause the cartilage to thin, become rough and lose its elasticity. As the underlying bone tissue grows, the joint space narrows and osteophytes form - marginal growths. The synovium thickens, the ligaments thicken and shorten, and muscle function is impaired.
The pathological process in the joint develops gradually, but does not go without a trace. Disorders of cartilage and other structures inevitably affect the clinical manifestations of osteoarthritis.
Classification
Like other diseases, there are certain types of joint diseases. This must be taken into account in the clinical classification of the disease. The pathology is primary when it develops in healthy joints and secondary if it arises in the context of other diseases. In the absence of a cause, they say idiopathic osteoarthritis. Depending on the number of joints involved, the following varieties can be distinguished:
- Monoarticular disease.
- Fewer joints - no more than 2 joints are affected.
- Polyarthropathy - involves 3 joint groups.
If the pathological process is universal, then we can talk about the failure of almost all joints of the body, including the spine where spondyloarthropathies are observed. In this case, the disease can progress in the form of nodules or nodules.
It is important to understand the processes that take place in the joints and to fully assess their severity. Therefore, the stage of arthropathy must be taken into account. It does not depend on the cause and is determined by the pathological changes in the joint tissue:
- Stage 1 - The synovium becomes inflamed and the cartilage loses its ability to bear the load.
- Stage 2 - Cartilage tissue destruction, bone growth, joint pocket dystrophy.
- Stage 3 - Skeletal deformities, contractures, joint instability.
The presence of signs of inflammation should also be reflected in the classification. Therefore, osteoarthritis is distinguished from synovitis with and without synovitis. In addition, the functional status of the joint is also important, depending on the degree of insufficiency:
- 1 degree - Temporarily limited functionality.
- Level 2 - Disability.
- 3rd degree - Impossible for self-service.
All of these features should be reflected in the diagnosis of osteoarthritis because they are important for subsequent treatment.
symptom

In joint pathology, the symptoms of arthropathy are quite distinct. They develop gradually but steadily, resulting in limited physical activity in patients. Therefore, it is particularly important to suspect the disease in a timely manner in order to be able to stop its development and prevent complications.
When contacting a doctor, first analyze the patient's complaint. Most people worry about joint pain. But with arthropathy, unlike other diseases like arthritis, they have the following characteristics:
- Mechanical - Occurs in the context of load and decreases at rest.
- Onset - The onset of pain is associated with the onset of movement (walking).
- "Joint rat" - Periodic severe pain with joint blockage caused by damage to the synovium between the cartilage surfaces.
At first, patients may experience only vague joint discomfort, accompanied by fatigue. But over time, it can develop into pain. If in the initial phase it worries after load, then in the future - during exercise, in advanced situations it becomes constant, even at rest and at night.
In addition to pain, patients have other symptoms of arthropathy. They are subjective and objective, with the following characteristics:
- Joint stiffness in the morning for no more than 30 minutes.
- There is a crunching feeling (crepitus) when moving.
- The area around the joint is deformed.
- Limit mobility.
For hand arthropathy, during examination, one can notice the characteristic formation of the proximal and distal phalangeal regions - Bouchard's and Heberden's nodes. Feeling the affected joint is often painful. If a contracture develops, some parts of the extremity are more often fixed in a flexed position.
The remarkable nature of osteoarthritis results in a significant decrease in the patient's level of physical activity, which in turn leads to a decrease in their quality of life.
diagnosis
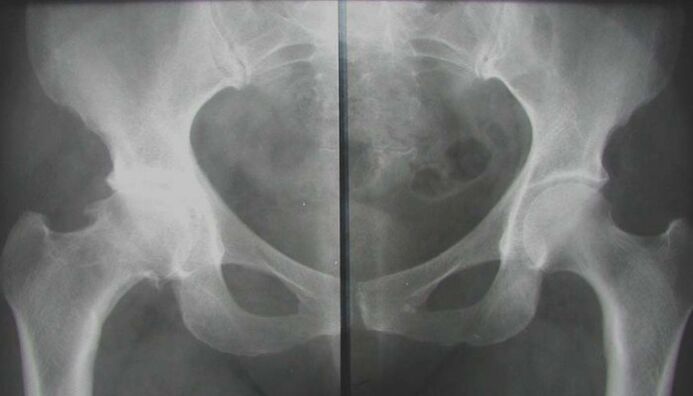
To understand why the clinical manifestations develop, it is necessary to confirm the pathology of the joint. This can be done by performing the necessary diagnostic tests, which include instrumentation and laboratory methods. First, they sought to see structural changes in affected areas to assess their severity and prevalence. There is also a need to identify metabolic disturbances in vivo, which have become a favorable background for the development of arthropathy. Therefore, the survey complex includes the following activities:
- radiography.
- Magnetic resonance imaging.
- Ultrasound program.
- Arthroscopy.
- Biochemical blood tests (hormone profile, inflammatory markers, calcium metabolism, rheumatology).
After the examination, it is necessary to consult an orthopaedic surgeon-traumatologist, which will help to develop the correct treatment strategy for each patient.
treat

Arthropathy requires comprehensive treatment. This means that all available therapeutics are used to relieve the patient's condition. But you need to understand that their effectiveness is directly dependent on the duration of treatment. For advanced forms of the disease, conservative measures are of little help. Early treatment can lead to clear and long-lasting results. For the treatment of osteoarthritis, use the following methods:
- medical treatment.
- physiotherapy.
- physiotherapy.
- massage.
- Operation.
What funding is right for a particular patient is up to the doctor. Selection is made based on examination results and individual characteristics of the organism.
Treatment is best when correction is initiated in the early stages of the disease, when the first symptoms are just beginning to appear.
General advice
Since the development of joint degenerative changes is mediated by increased loading, there is a first need to reduce mechanical effects on cartilage tissue. To do this, you should stop doing heavy, intense exercise training. To unload the joint, any method works - from walking on crutches to special fixed orthoses. But it is impossible to give up exercise entirely, and physical activity should be pursued. Useful for short walks and swimming.
Proper nutrition plays an important role in correcting joint pathologies. Diet helps improve the condition of cartilage, but is also a major ingredient in combating excess weight. Advise patients to eat lean meat and poultry, fish, and cereals; you need to enrich your diet with fresh vegetables and fruits, and herbs. But in return, you should avoid smoky, spicy, greasy foods, marinades, and pickles. Best to watch out for foods rich in collagen fibers, elastin, and gelatin: aspic, hash, aspic dishes, jellies.
medical treatement

Traditional treatment of osteoarthritis begins with medication. Using various drugs, it is possible not only to eliminate the symptoms of the disease, but also to influence the mechanism of its development. This is especially important in chronic degenerative joint pathology, where structural modification of cartilage tissue is required. The following drugs are generally recommended:
- Non-steroidal anti-inflammatory drugs.
- chondroprotective agent.
- Blood vessel.
- Vitamins and Antioxidants.
- Metabolism (estrogen, thyroid hormones).
In severe joint pain, intra-articular glucocorticoid injections may be administered. But this treatment should be short-term because long-term use of hormonal drugs can have the opposite effect - they stimulate the process of malnutrition. Systemic therapy should be combined with topical medications.
Take medication for osteoarthritis as recommended by your doctor and under his control. No medication is allowed on its own.
physiotherapy
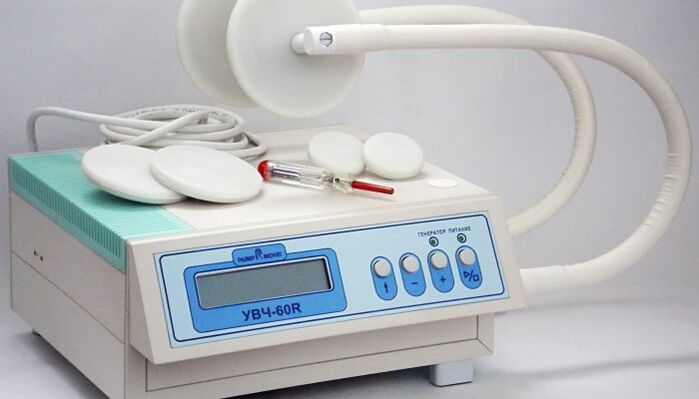
Methods of physical influence help to eliminate acute symptoms of joint pathology. Together with drugs, they can reduce the severity of pain and inflammation, and they can also stimulate biochemical processes in the cartilage itself. In the complex treatment of arthropathy, the following procedures are used:
- electrophoresis.
- Ultrasonic treatment.
- Wave therapy.
- Magnetic therapy.
- Laser Treatment.
- Mud and spa.
This method affects not only the joints, but also the surrounding tissue. This helps activate blood circulation, improve nutritional processes and weaken muscle contractures. Many elements of spa treatments have general health-improving effects. But at the same time, the contraindications of physiotherapy should not be forgotten: infectious diseases, tumors, cardiovascular diseases, renal failure, bleeding, serious condition of the patient.
physiotherapy
An important aspect of non-drug therapy for osteoarthritis is exercise therapy. It is well known that the metabolism of cartilage tissue is significantly dependent on mechanical factors. But his strength must be sufficient. Only then can the growth process overcome destruction. Therefore, gymnastics is suitable for all patients with joint diseases. But for each individual, their own set of exercises is developed - taking into account the location and severity of the lesions, as well as the general condition of the body.
Pain should not be allowed to arise during the class. Exercise at a slow pace only after acute symptoms have resolved. Avoid sudden and high-amplitude movements that may cause discomfort. Physical education classes should be conducted under the guidance of a doctor, and once you have mastered the necessary skills, you can start exercising at home.
Therapeutic gymnastics is an integral part of the process of correcting degenerative joint dystrophy. Only regular courses have positive results.
massage

To improve the condition of the musculoskeletal system, massage sessions are shown. Manual shocks to your joints allow you to relax spasmodic muscle groups, stimulate circulation in soft tissues, and prepare you for active exercise (before therapeutic exercise). Classical massage includes the following elements:
- stroking.
- Grind.
- knead.
- pressure.
- Iron.
It is usually combined with passive movement of the affected joint. The duration of treatment is determined by the doctor and can range from 7 to 15 sessions.
Operation
Surgical treatment is required if the desired results cannot be achieved with conservative measures in the advanced stages of osteoarthritis. Its essence is to use artificial joint replacement - arthroplasty. The surgery is performed openly and under general anesthesia. Once done, you need to start rehab as early as possible. Thanks to the surgical intervention, the patient can completely get rid of the arthropathy and return to an active life. Granted, this action is not available to everyone.
Osteoarthritis is a common problem that requires prompt and aggressive solutions. Treatment should be started as early as possible in order not to start the disease and to be able to hope that conservative measures will be successful. This will avoid deterioration, prevent the progression of joint changes, and restore the functional capacity of the musculoskeletal system as much as possible. Otherwise, surgical correction must be considered.
























